Search
- Page Path
- HOME > Search
- Hypothalamus and Pituitary Gland
- Metabolic Impacts of Discontinuation and Resumption of Recombinant Human Growth Hormone Treatment during the Transition Period in Patients with Childhood-Onset Growth Hormone Deficiency
- Yun Jeong Lee, Yunha Choi, Han-Wook Yoo, Young Ah Lee, Choong Ho Shin, Han Saem Choi, Ho-Seong Kim, Jae Hyun Kim, Jung Eun Moon, Cheol Woo Ko, Moon Bae Ahn, Byung-Kyu Suh, Jin-Ho Choi
- Endocrinol Metab. 2022;37(2):359-368. Published online April 25, 2022
- DOI: https://doi.org/10.3803/EnM.2021.1384

- 4,464 View
- 185 Download
- 3 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Discontinuing growth hormone (GH) treatment during the transition to adulthood has been associated with adverse health outcomes in patients with childhood-onset growth hormone deficiency (CO-GHD). This study investigated the metabolic changes associated with interrupting GH treatment in adolescents with CO-GHD during the transition period.
Methods
This study included 187 patients with CO-GHD who were confirmed to have adult GHD and were treated at six academic centers in Korea. Data on clinical parameters, including anthropometric measurements, metabolic profiles, and bone mineral density (BMD) at the end of childhood GH treatment, were collected at the time of re-evaluation for GHD and 1 year after treatment resumption.
Results
Most patients (n=182, 97.3%) had organic GHD. The median age at treatment discontinuation and re-evaluation was 15.6 and 18.7 years, respectively. The median duration of treatment interruption was 2.8 years. During treatment discontinuation, body mass index Z-scores and total cholesterol, low-density lipoprotein, and non-high-density lipoprotein (HDL) cholesterol levels increased, whereas fasting glucose levels decreased. One year after GH treatment resumption, fasting glucose levels, HDL cholesterol levels, and femoral neck BMD increased significantly. Longer GH interruption (>2 years, 60.4%) resulted in worse lipid profiles at re-evaluation. The duration of interruption was positively correlated with fasting glucose and non-HDL cholesterol levels after adjusting for covariates.
Conclusion
GH treatment interruption during the transition period resulted in worse metabolic parameters, and a longer interruption period was correlated with poorer outcomes. GH treatment should be resumed early in patients with CO-GHD during the transition period. -
Citations
Citations to this article as recorded by- Ghrelin regulating liver activity and its potential effects on liver fibrosis and Echinococcosis
Jiang Zhu, Tanfang Zhou, Meng Menggen, Kalibixiati Aimulajiang, Hao Wen
Frontiers in Cellular and Infection Microbiology.2024;[Epub] CrossRef - Composición de la microbiota en pacientes con déficit de hormona de crecimiento antes y después de recibir tratamiento
Patricia García Navas, María Yolanda Ruíz del Prado, Pablo Villoslada Blanco, Emma Recio Fernández, María Ruíz del Campo, Patricia Pérez Matute
Anales de Pediatría.2024;[Epub] CrossRef - Relationship between the Stimulated Peak Growth Hormone Level and Metabolic Parameters in Children with Growth Hormone Deficiency
Seong Yong Lee
The Ewha Medical Journal.2023;[Epub] CrossRef - Dyslipidaemia and growth hormone deficiency – A comprehensive review
Matthias Hepprich, Fahim Ebrahimi, Emanuel Christ
Best Practice & Research Clinical Endocrinology & Metabolism.2023; 37(6): 101821. CrossRef
- Ghrelin regulating liver activity and its potential effects on liver fibrosis and Echinococcosis

- Miscellaneous
- Diagnosis and Treatment of Growth Hormone Deficiency: A Position Statement from Korean Endocrine Society and Korean Society of Pediatric Endocrinology
- Jung Hee Kim, Hyun Wook Chae, Sang Ouk Chin, Cheol Ryong Ku, Kyeong Hye Park, Dong Jun Lim, Kwang Joon Kim, Jung Soo Lim, Gyuri Kim, Yun Mi Choi, Seong Hee Ahn, Min Ji Jeon, Yul Hwangbo, Ju Hee Lee, Bu Kyung Kim, Yong Jun Choi, Kyung Ae Lee, Seong-Su Moon, Hwa Young Ahn, Hoon Sung Choi, Sang Mo Hong, Dong Yeob Shin, Ji A Seo, Se Hwa Kim, Seungjoon Oh, Sung Hoon Yu, Byung Joon Kim, Choong Ho Shin, Sung-Woon Kim, Chong Hwa Kim, Eun Jig Lee
- Endocrinol Metab. 2020;35(2):272-287. Published online June 24, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.2.272
- 9,528 View
- 429 Download
- 14 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
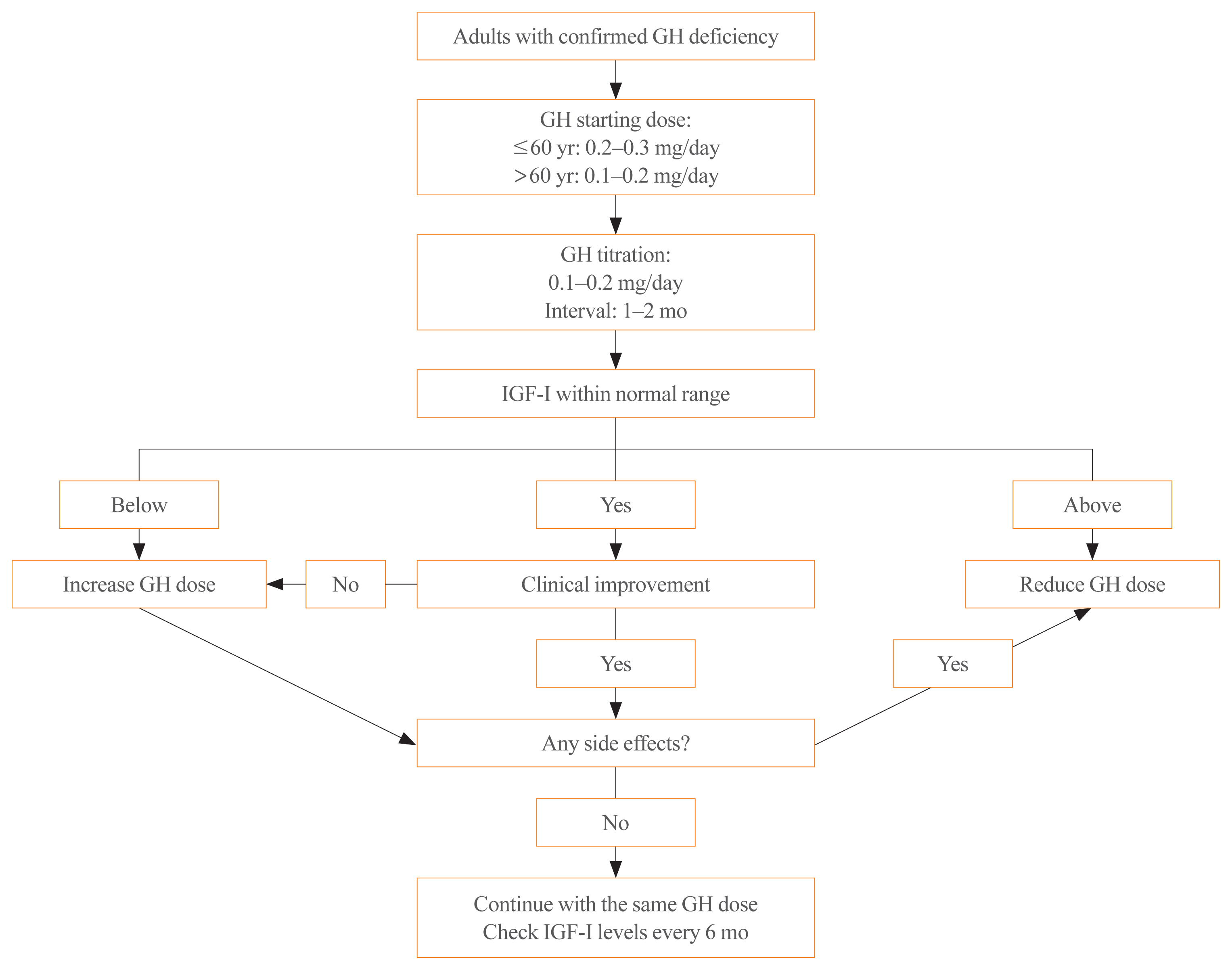
ePub - Growth hormone (GH) deficiency is caused by congenital or acquired causes and occurs in childhood or adulthood. GH replacement therapy brings benefits to body composition, exercise capacity, skeletal health, cardiovascular outcomes, and quality of life. Before initiating GH replacement, GH deficiency should be confirmed through proper stimulation tests, and in cases with proven genetic causes or structural lesions, repeated GH stimulation testing is not necessary. The dosing regimen of GH replacement therapy should be individualized, with the goal of minimizing side effects and maximizing clinical improvements. The Korean Endocrine Society and the Korean Society of Pediatric Endocrinology have developed a position statement on the diagnosis and treatment of GH deficiency. This position statement is based on a systematic review of evidence and expert opinions.
-
Citations
Citations to this article as recorded by- Once-Weekly Somapacitan as an Alternative Management of Growth Hormone Deficiency in Prepubertal Children: A Systematic Review and Meta-Analysis of Randomized Controlled Trial
Ghina Tsurayya, Cut Alifiya Nazhifah, Muhammad Rahmat Pirwanja, Putri Oktaviani Zulfa, Muhammad Raihan Ramadhan Tatroman, Fajar Fakri, Muhammad Iqhrammullah
Children.2024; 11(2): 227. CrossRef - Efficacy, safety, and patient satisfaction of norditropin and sogroya in patients with growth hormone deficiency: a systematic review and meta-analysis of randomized controlled trials
Obieda Altobaishat, Mohamed Abouzid, Mostafa Hossam El Din Moawad, Abdulrahman Sharaf, Yazan Al-Ajlouni, Tungki Pratama Umar, Abdallah Bani-salameh, Mohammad Tanashat, Omar Abdullah Bataineh, Abdulqadir J. Nashwan
Endocrine.2024;[Epub] CrossRef - Evaluation of Adult Height in Patients with Non-Permanent Idiopathic GH Deficiency
Agnese Murianni, Anna Lussu, Chiara Guzzetti, Anastasia Ibba, Letizia Casula, Mariacarolina Salerno, Marco Cappa, Sandro Loche
Endocrines.2023; 4(1): 169. CrossRef - The effect of hypothalamic involvement and growth hormone treatment on cardiovascular risk factors during the transition period in patients with childhood-onset craniopharyngioma
Sang Hee Park, Yun Jeong Lee, Jung-Eun Cheon, Choong Ho Shin, Hae Woon Jung, Young Ah Lee
Annals of Pediatric Endocrinology & Metabolism.2023; 28(2): 107. CrossRef - Continuous Glucose Monitoring: A Possible Aid for Detecting Hypoglycemic Events during Insulin Tolerance Tests
Soo Yeun Sim, Moon Bae Ahn
Sensors.2023; 23(15): 6892. CrossRef - The risk patients with AGHD have of developing CVD
Eisha Javed, Maha Zehra, Naz Elahi
International Journal of Cardiology Cardiovascular Risk and Prevention.2023; 19: 200221. CrossRef - Diagnosis of GH Deficiency Without GH Stimulation Tests
Anastasia Ibba, Sandro Loche
Frontiers in Endocrinology.2022;[Epub] CrossRef - Metabolic Impacts of Discontinuation and Resumption of Recombinant Human Growth Hormone Treatment during the Transition Period in Patients with Childhood-Onset Growth Hormone Deficiency
Yun Jeong Lee, Yunha Choi, Han-Wook Yoo, Young Ah Lee, Choong Ho Shin, Han Saem Choi, Ho-Seong Kim, Jae Hyun Kim, Jung Eun Moon, Cheol Woo Ko, Moon Bae Ahn, Byung-Kyu Suh, Jin-Ho Choi
Endocrinology and Metabolism.2022; 37(2): 359. CrossRef - A Radiomics-Based Model with the Potential to Differentiate Growth Hormone Deficiency and Idiopathic Short Stature on Sella MRI
Taeyoun Lee, Kyungchul Song, Beomseok Sohn, Jihwan Eom, Sung Soo Ahn, Ho-Seong Kim, Seung-Koo Lee
Yonsei Medical Journal.2022; 63(9): 856. CrossRef - Phenotypic spectrum of patients with mutations in CHD7: clinical implications of endocrinological findings
Ja Hye Kim, Yunha Choi, Soojin Hwang, Gu-Hwan Kim, Han-Wook Yoo, Jin-Ho Choi
Endocrine Connections.2022;[Epub] CrossRef - Immune Checkpoint Inhibitors and Endocrine Disorders: A Position Statement from the Korean Endocrine Society
Hyemi Kwon, Eun Roh, Chang Ho Ahn, Hee Kyung Kim, Cheol Ryong Ku, Kyong Yeun Jung, Ju Hee Lee, Eun Heui Kim, Sunghwan Suh, Sangmo Hong, Jeonghoon Ha, Jun Sung Moon, Jin Hwa Kim, Mi-kyung Kim
Endocrinology and Metabolism.2022; 37(6): 839. CrossRef - Laron syndrome: clinic, diagnostics (а clinical case)
P.M. Lіashuk, R.P. Lіashuk, N.I. Stankova, M.B. Kudina
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2022; 18(3): 193. CrossRef - Diagnosis for Pheochromocytoma and Paraganglioma: A Joint Position Statement of the Korean Pheochromocytoma and Paraganglioma Task Force
Eu Jeong Ku, Kyoung Jin Kim, Jung Hee Kim, Mi Kyung Kim, Chang Ho Ahn, Kyung Ae Lee, Seung Hun Lee, You-Bin Lee, Kyeong Hye Park, Yun Mi Choi, Namki Hong, A Ram Hong, Sang-Wook Kang, Byung Kwan Park, Moon-Woo Seong, Myungshin Kim, Kyeong Cheon Jung, Chan
Endocrinology and Metabolism.2021; 36(2): 322. CrossRef - Asian Conference on Tumor Ablation Guidelines for Adrenal Tumor Ablation
Byung Kwan Park, Masashi Fujimori, Shu-Huei Shen, Uei Pua
Endocrinology and Metabolism.2021; 36(3): 553. CrossRef - Asian Conference on Tumor Ablation guidelines for renal cell carcinoma
Byung Kwan Park, Shu-Huei Shen, Masashi Fujimori, Yi Wang
Investigative and Clinical Urology.2021; 62(4): 378. CrossRef - Diagnosis and Treatment of Adult Growth Hormone Deficiency
Jung Hee Kim
The Korean Journal of Medicine.2021; 96(5): 400. CrossRef
- Once-Weekly Somapacitan as an Alternative Management of Growth Hormone Deficiency in Prepubertal Children: A Systematic Review and Meta-Analysis of Randomized Controlled Trial

- Clinical Study
- Effects of Maternal Iodine Status during Pregnancy and Lactation on Maternal Thyroid Function and Offspring Growth and Development: A Prospective Study Protocol for the Ideal Breast Milk Cohort
- Young Ah Lee, Sun Wook Cho, Ho Kyung Sung, Kyungsik Kim, Young Shin Song, Sin Je Moon, Jung Won Oh, Dal Lae Ju, Sooyeon Choi, Sang Hoon Song, Gi Jeong Cheon, Young Joo Park, Choong Ho Shin, Sue K. Park, Jong Kwan Jun, June-Key Chung
- Endocrinol Metab. 2018;33(3):395-402. Published online September 18, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.3.395
- 4,961 View
- 84 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Iodine is an intrinsic element of thyroid hormone, which is essential for childhood growth and development. The Ideal Breast Milk (IBM) cohort study aims to evaluate the effects of maternal iodine status during pregnancy and lactation on maternal thyroid function, offspring growth and development, and offspring thyroid function.
Methods The IBM cohort study recruited pregnant women from Seoul National University Hospital between June 2016 and August 2017, followed by enrollment of their offspring after delivery. For the maternal participants, iodine status is evaluated by urinary iodine concentration (UIC) and dietary records in the third trimester and at 3 to 4 weeks and 12 to 15 months postpartum. For the child participants, cord blood sampling and UIC measurements are performed at birth. At 3 to 4 weeks of age, UIC and breastmilk iodine concentrations are measured. At 12 to 15 months of age, growth and development are assessed and measurements of UIC, a thyroid function test, and ultrasonography are performed.
Results A total of 198 pregnant women in their third trimester were recruited. Their mean age was 35.1±3.5 years, and 78 (39.4%) of them were pregnant with twins. Thirty-three (16.7%) of them had a previous history of thyroid disease.
Conclusion Korea is an iodine-replete area. In particular, lactating women in Korea are commonly exposed to excess iodine due to the traditional practice of consuming brown seaweed soup postpartum. The study of the IBM cohort is expected to contribute to developing guidelines for optimal iodine nutrition in pregnant or lactating women.
-
Citations
Citations to this article as recorded by- High intakes of iodine among women during pregnancy and the postpartum period has no adverse effect on thyroid function
Dal Lae Ju, Sun Wook Cho, Chae Won Chung, Young Ah Lee, Gi Jeong Cheon, Young Joo Park, Choong Ho Shin, Jong Kwan Jun, June-Key Chung, Sue K. Park, YoonJu Song
European Journal of Nutrition.2023; 62(1): 239. CrossRef - Associations between maternal thyroid function in pregnancy and child neurodevelopmental outcomes at 20 months in the Seychelles Child Development Study, Nutrition Cohort 2 (SCDS NC2)
Anna M. Monaghan, Maria S. Mulhern, Emeir M. Mc Sorley, J.J. Strain, Theresa Winter, Edwin van Wijngaarden, Gary J. Myers, Philip W. Davidson, Conrad Shamlaye, Jude Gedeon, Alison J. Yeates
Journal of Nutritional Science.2021;[Epub] CrossRef
- High intakes of iodine among women during pregnancy and the postpartum period has no adverse effect on thyroid function

- Clinical Characteristics of Langerhans Cell Histiocytosis with Hypothalamo-Pituitary Involvement.
- Eun Shil Hong, Jung Hun Ohn, Jung Hee Kim, Yul Hwang-Bo, Jin Joo Kim, Jung Hee Kwon, Jung Won Lee, Se Youn Choi, Eun Kyung Lee, Sun Wook Cho, Chan Soo Shin, Kyong Soo Park, Hak Chul Jang, Bo Youn Cho, Hong Kyu Lee, Choong Ho Shin, Sei Won Yang, Seong Yeon Kim
- Endocrinol Metab. 2011;26(1):38-43. Published online March 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.1.38
- 1,949 View
- 23 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Langerhans cell histiocytosis (LCH) is a rare disease that involves a clonal proliferation of Langerhans cells. LCH has a predilection for hypothalamo-pituitary axis (HPA) dysfunction, and this leads to diabetes insipidus (DI) and/or anterior pituitary dysfunction. Here, we describe the endocrine dysfunction and clinical characteristics of adult patients with LCH and we analyzed the differences between an adult-onset type and a childhood-onset type. METHODS: The data was obtained from a retrospective chart review of the patients with LCH that involved the HPA and who attended Seoul National University Hospital. The patients were classified into the adult-onset type (age at the time of diagnosis > or = 16) and the childhood-onset type (age at the time of diagnosis < or = 15). RESULTS: Ten patients (9 males and 1 female) were diagnosed with LCH involving the HPA. Five patients were classified as an adultonset type and the other five patients were classified as a childhood-onset type. The median follow-up duration was 6 (3-12) years for the adult-onset type and 16 (15-22) years for the childhood-onset type. All the patients presented with DI as the initial manifestation of HPA involvement. Four adult-onset patients and three childhood-onset patients had a multi-system disease. Panhypopituitarism developed in three adult-onset patients and in one childhood-onset patient. The pituitary lesion of the three adult-onset patients had spread to the brain during the follow-up duration. In contrast, the pituitary lesion of the other two adult-onset patients without panhypopituitarism and all the childhood-onset patients had not changed. CONCLUSION: DI was the initial presentation symptom of HPA involvement. Anterior pituitary hormone deficiency followed in some patients. Compared with the childhood-onset patients, the adult-onset patients were more likely to have panhypopituitarism and a poor prognosis. -
Citations
Citations to this article as recorded by- Pulmonary Langerhans Cell Histiocytosis in an Adult Male Presenting with Central Diabetes Insipidus and Diabetes Mellitus: A Case Report
Yeun Seoung Choi, Jung Soo Lim, Woocheol Kwon, Soon-Hee Jung, Il Hwan Park, Myoung Kyu Lee, Won Yeon Lee, Suk Joong Yong, Seok Jeong Lee, Ye-Ryung Jung, Jiwon Choi, Ji Sun Choi, Joon Taek Jeong, Jin Sae Yoo, Sang-Ha Kim
Tuberculosis and Respiratory Diseases.2015; 78(4): 463. CrossRef - Adult Multisystem Langerhans Cell Histiocytosis Presenting with Central Diabetes Insipidus Successfully Treated with Chemotherapy
Jung-Eun Choi, Hae Ri Lee, Jung Hun Ohn, Min Kyong Moon, Juri Park, Seong Jin Lee, Moon-Gi Choi, Hyung Joon Yoo, Jung Han Kim, Eun-Gyoung Hong
Endocrinology and Metabolism.2014; 29(3): 394. CrossRef
- Pulmonary Langerhans Cell Histiocytosis in an Adult Male Presenting with Central Diabetes Insipidus and Diabetes Mellitus: A Case Report


 KES
KES

 First
First Prev
Prev



